Pag-unawa sa Biotherapy at ang Papel Nito sa Regulasyon ng Imyunong Balat
Kahulugan at Saklaw ng Biotherapy sa Dermatolohiya
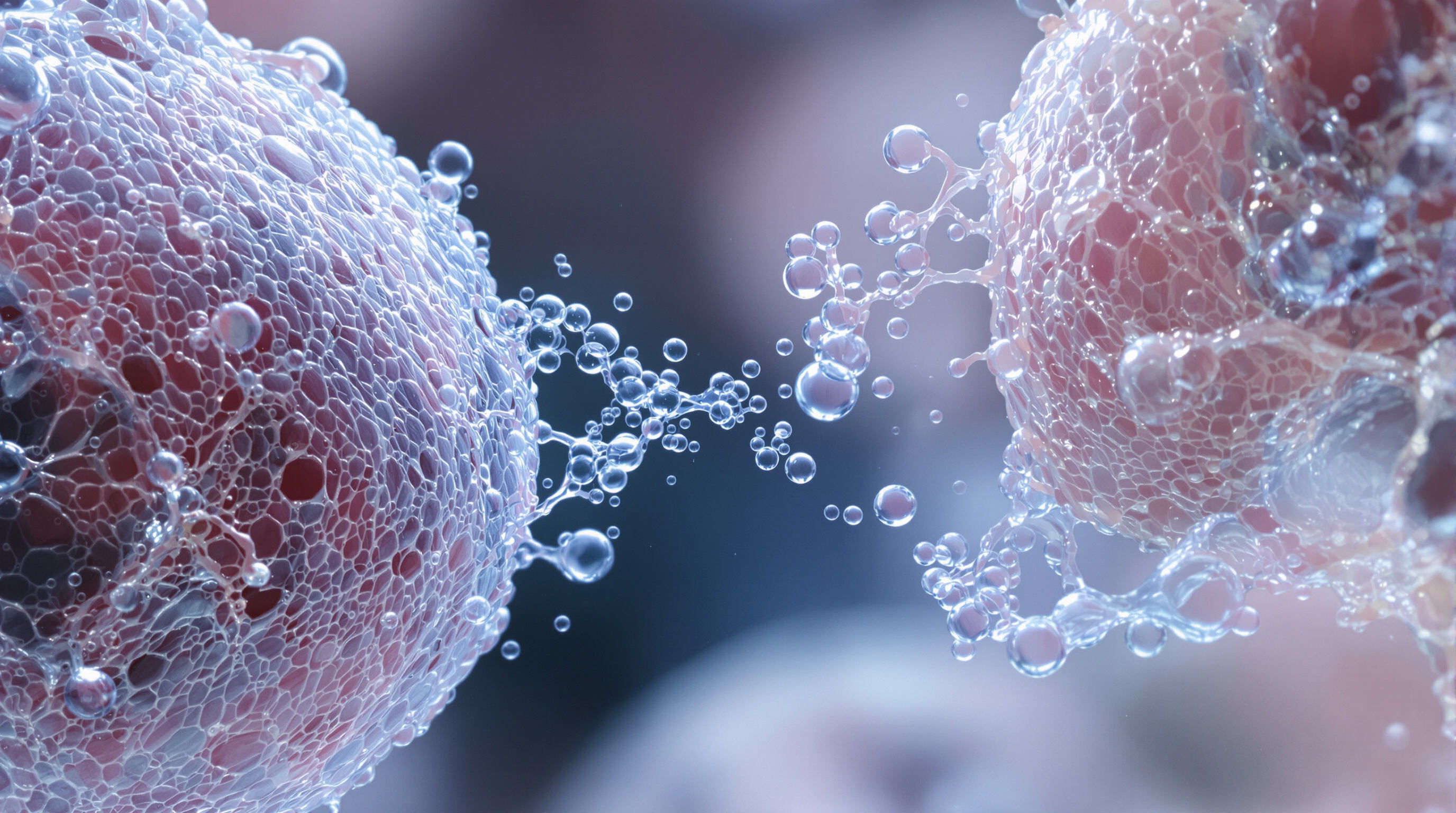
Ang biotherapy ay gumagana sa pamamagitan ng paggamit ng mga substansya mula sa mga buhay na organismo tulad ng mga protina, growth factors, at mga maliit na bahagi ng selulang tinatawag na exosomes upang tugunan ang mga pangmatagalang problema sa balat kabilang ang eksema, psoriasis, at sintomas ng pinsalang dulot ng araw. Ang tradisyonal na paggamot ay karamihan ay nagtatago lamang sa mga sintomas, samantalang ang biotherapy ay direktang tumatalakay sa tunay na ugat ng maraming kondisyon sa balat—ang mga problema sa paraan ng paggana ng imyunong sistema. Isang pananaliksik noong 2022 mula sa journal na Frontiers in Bioengineering and Biotechnology ay nagpakita ng isang kahanga-hangang resulta: sa pagtrato sa psoriasis na dulot ng autoimyunidad, ang biotherapy ay binawasan ang mga pagbalik ng sakit ng humigit-kumulang isang ikatlo kumpara sa karaniwang paggamot gamit ang steroid ayon sa pag-aaral nina Bellei at kasama noong nakaraang taon. Ito ay nagmumungkahi na ang biotherapy ay maaaring talagang makatulong sa pangmatagalang pamamahala ng mga kondisyong ito imbes na magbigay lamang ng pansamantalang lunas.
Papel ng Mga Bioaktibong Kadahilanan sa Pagbabago ng Imyunong Balat
Ang mga bioactive na sangkap na ginamit sa biotherapy ay nakikialam sa mahahalagang landas ng immune system sa pamamagitan ng pagpapanatiling balanse ang antas ng cytokine (tulad ng TNF-alpha, IL-6, at IL-10) habang dinadalian nito ang pag-uugali ng mga macrophage (kung sila ba ay kumikilos bilang M1 o M2 na uri). Kung paparating sa exosomes mula sa mesenchymal stem cells, ang mga maliit na partikulong ito ay dala ang microRNAs na humahadlang sa NF-kappa B signaling pathway, na labis na aktibo tuwing magkakaroon ng pagsulpot ng eksema. Ayon sa pag-aaral noong 2019 nina Wang at kasama, napapatunayan na mas mabilis ng 21 porsiyento ang paggaling ng barrier ng balat gamit ang paraang ito kumpara sa tradisyonal na topical treatments tulad ng calcineurin inhibitors.
Ugnayan sa Pagitan ng Regenerative Medicine at Skin Immune Defense
Ang regeneratibong biotherapy ay gumagawa ng mga kababalaghan para sa natural na proseso ng pagpapagaling sa pamamagitan ng pag-aktibo sa mga stem cell na ginawa ng katawan. Ang mga paggamot na galing sa mesenchymal stem cells ay higit pa sa simpleng pagpapatahimik ng pamamaga; ito ay aktwal na tumutulong sa pagbuo ng bagong collagen at sa pagsasaayos muli ng mga nasirang tisyu sa pamamagitan ng mga kemikal na senyas sa pagitan ng mga selula. Ayon sa pangkat ni Paganelli noong 2020, ang ilang kamakailang pag-aaral ay nakakita na ang pagsasama ng mga terapiyang batay sa selula kasama ang mga espesyal na materyales na idinisenyo upang gayahin ang mga biyolohikal na istruktura ay nagpabuti ng paggaling ng sugat ng humigit-kumulang 40%. Ang kombinasyong ito ay tila partikular na epektibo sa pagpapalakas ng kakayahan ng balat na labanan ang impeksyon at mag-repair pagkatapos ng pinsala.
Mga Bio-factor at Inter-cellular na Komunikasyon sa Pamamagitan ng Extracellular Vesicles
Mga Exosome sa Pagtanda ng Balat at Photoaging: Mga Mekanismo ng Inter-cellular na Pagpapadala ng Senyas
Ang mga maliit na partikulo ng exosome ay gumagana nang parang mensahero sa pagitan ng mga selula parehong sa normal na pagtanda at sa balat na nasugatan ng araw. Dala nila ang lahat ng uri ng bagay kabilang ang mga protina, taba, at mga maliit na RNA fragment upang tulungan ayusin ang mga bagay sa antas ng selula. Ang ilang kamakailang pag-aaral mula sa Journal of Nanobiotechnology noong 2023 ay nakita na ang mga exosome ay talagang tumutulong labanan ang oxidative stress sa pamamagitan ng pagdadala ng catalase enzymes. Ang mga pagsusuri ay nagpakita na nabawasan nito ang pinsala ng UV sa mga selula ng balat ng tao ng halos 40 porsiyento. Higit pa rito, ang mga exosome ding ito ang nagdadala ng TGF-beta signals na nagsisimula sa proseso ng paggawa ng collagen sa loob ng balat. Nakakatulong ito upang labanan ang pagkasira ng mga network na sumusuporta sa istruktura na natural na nangyayari habang tumatanda tayo.
Mga Exosome na Galing sa Stem Cell at ang Kanilang Potensyal na Terapeutiko sa Pagbabago ng Imapre
Ang exosome ng mesenkimal na stem cell ay nagbibigay ng dual-phase na immune modulation: una'y pinipigilan ang labis na pamamaga sa pamamagitan ng IL-10 delivery, at pagkatapos ay tinutulungan ang pagkukumpuni ng tisyu sa pamamagitan ng macrophage activation. Sa mga klinikal na modelo, ang mga eksomang ito ay nagpapabalik ng skin barrier nang 63% na mas mabilis kaysa sa tradisyonal na growth factor serums, na siya pong ideal para sa mga biotherapy protocol na target ang immune dysregulation.
Mesenchymal Stem Cells (MSCs) at Ang Kanilang Paracrine Effects sa Pagkukumpuni ng Balat
Inilalabas ng mga stem cell ang mga maliit na pakete na tinatawag na extracellular vesicles na naglalaman ng higit sa 150 iba't ibang aktibong sangkap. Kabilang dito ang TIMP inhibitors na humihinto sa mga MMP enzymes na sirain ang collagen fibers. Kapag inilapat sa balat na nasugatan dahil sa araw, ang mga vesicle na ito ay pinalakas ang produksyon ng type I collagen ng humigit-kumulang 29% pagkalipas lamang ng walong linggo. Nang magkatime, binawasan nila ang antas ng TNF alpha ng mga 41 porsyento. Ano ang resulta? Regenerasyon ng balat na katulad ng nangyayari kapag direktang itinatransplanta ang mga stem cell, ngunit walang mga potensyal na komplikasyon na kasama ng tunay na therapy gamit ang cells.
Biomimetic Biomaterials na Pina-enhance ang Pagpapadala ng Extracellular Vesicle
Ang mga thermoresponsive na tagapagdala ng hydrogel ay nagpapalawig ng bioavailability ng mga extracellular vesicle hanggang sa 300%, na nagbibigay-daan sa patuloy na paglabas ng mga regenerative na sangkap. Isang sistema noong 2023 batay sa hydrogel ang nagpakita ng 82% mas mataas na pag-absorb ng fibroblast sa malalim na dermal na layer kumpara sa libreng EVs, na pinagsasama ang suporta sa istruktura at marunong na paghahatid ng kargamento upang mapataas ang pagpapagaling ng immune system ng balat.
Mga Epekto sa Imyunomodulasyon ng mga Bio-factor sa Mga Nakakahawang Kondisyon ng Balat
Oxidative Stress at Paninilawan sa Pagtanda ng Balat: Pagtuon gamit ang Biotherapy
Kapag ang mga selula ay nakararanas ng paulit-ulit na oxidative stress, ang kanilang sensitibong redox balance ay nalalabag. Nakita namin ang mga pag-aaral na nagpapakita na ang regular na pagkakalantad sa UV ay maaaring mapataas ang antas ng reactive oxygen species (ROS) ng humigit-kumulang 38% ayon sa isang pag-aaral na nailathala sa Frontiers in Medicine noong nakaraang taon. Dito pumasok ang biotherapy, na parang nagpapadala ng mga antioxidant enzyme tulad ng superoxide dismutase upang labanan ang mga nakakalasong molekyul ng ROS. Ang mga enzyme na ito ay hindi lang humihinto doon—aktibo rin silang pinipigilan ang mga senyas ng NF-kappa B na nagdudulot ng malaking pinsala. Ang nagpapabisa sa paraang ito ay ang kakayahan nitong panatilihing maayos ang paggana ng mitochondria habang binabawasan ang lipid peroxidation ng halos dalawang ikatlo. Ano ang resulta? Mas malusog na nananatiling balat sa mas mahabang panahon dahil hindi na nawawala ang collagen sa dating bilis at hindi masyadong napapalitan ang ating panlabas na layer dahil sa paulit-ulit na pinsalang dulot ng araw.
Regulasyon ng Cytokine (hal., TNF-α, IL-6, IL-10) sa pamamagitan ng Bio-factors
Ang mga bio-factor ay nagbabalanse muli sa mga network ng cytokine sa mga pamumula ng balat tulad ng psoriasis. Isang pag-aaral noong 2023 ang nakahanap na ang mga exosome mula sa halaman ay nagpapababa ng pro-inflammatory na TNF-α at IL-6 ng 52% habang itinaas ang anti-inflammatory na IL-10. Ang selektibong modulasyon na ito ay nakalulutas sa mga cytokine storm nang hindi nagiging sanhi ng malawakang immunosuppression, na nag-aalok ng mas ligtas na alternatibo sa mga sintetikong inhibitor sa pamamagitan ng tiyak na pagta-target sa pagkakaiba ng Th17 cell.
Pagbabago ng Makropayj (M1/M2) sa Pagkukumpuni ng Tisyu at ang Modulasyon Nito ng Biotherapy
Ang biotherapy ay nagtataguyod ng paglipat mula sa pro-inflammatory na M1 tungo sa mapagbago na M2 makropayj sa pamamagitan ng senyales ng extracellular vesicle. Ang mga biomaterial na galing sa MSC ay nagpapataas ng populasyon ng M2 ng 81% (ScienceDirect, 2023), na pinalalakas ang pagbabago ng tisyu sa pamamagitan ng sekresyon ng TGF-β1 at VEGF. Ang transisyon na ito ay nagpapabuti ng pagkakasara ng sugat ng 40% sa mga kronikong ulser at binabawasan ang panganib ng fibrosis na kaugnay sa matinding aktibidad ng M1.
Mga Mahahalagang Growth Factor at Endogenous na Landas ng Pagkukumpuni ng Balat

Mga Pangunahing Growth Factor at Cytokine sa Pagkukumpuni na Pinamamahalaan ng Biotherapy
Talagang umaangat ang larangan ng biotherapy salamat sa mga espesyal na senyales na molekula tulad ng EGF at TGF-beta na nakatutulong sa pagsimula ng mga proseso ng pagpapabago ng balat. Halimbawa, ang EGF ay talagang kayang paikutin ang mga sel na keratinocyte at fibroblasts ng humigit-kumulang 40% habang nagpapagaling ang sugat, ayon sa ilang pananaliksik na nailathala noong nakaraang taon sa Frontiers in Cell and Developmental Biology. Samantala, ang TGF-beta ay gumagana naman naiiba sa pamamagitan ng pagbabantay sa mga marker ng pamamaga tulad ng IL-6 habang tumutulong ito sa pagbawi ng extracellular matrix. At ngayon, nakikita na natin ang ilang kapani-paniwala pag-unlad sa mga bagong biomimetic na materyales na nararanasan sa merkado. Ang mga ito ay kadalasang gumaganap bilang mga tagapagpatatag para sa iba pang mga growth factor tulad ng FGF-7, na ipinakita na tumaas ang antas ng elastin ng humigit-kumulang 34% lalo na sa balat na nasira dahil sa matagal na pagkakalantad sa araw. Talagang kahanga-hanga kung tutuusin.
Pag-aktibo sa Endogenous na Pagpapabago ng Balat Gamit ang Bio-Factors
Ang mga bagong pag-unlad sa biotherapy ay nagpapabalik sa natural na proseso ng pagpapagaling ng balat sa pamamagitan ng pagtutuon sa pagre-repair ng pinsala sa mitochondria at pag-alis sa mga nakakaabala na reactive oxygen species na nagdudulot ng maraming problema. Halimbawa, ang mga exosome na nagmula sa fibroblast—ang mga maliit na mensaherong ito ay tila nagpapagsimula sa Nrf2 antioxidant pathway na ipinakita naman na nagpapababa ng mga marker ng oxidative stress ng halos 60% sa mas matandang mga sample ng balat. Ang nagpapabukod-tangi sa gamot na ito ay ang kakayahang ibalik ang normal na paggana ng sariling stem cell ng katawan habang tinutulungan din nitong muling itayo ang mga nasirang tisyu sa pamamagitan ng mas mahusay na regulasyon sa antas ng MMP-1 at paghikayat sa tamang pagbuo ng collagen III. Ang mga mananaliksik ay nakabuo rin ng matalinong paraan upang mas epektibong maipadala ang mga terapiyang ito. Nakilala rito ang thermoresponsive hydrogels dahil ito ay nagpapataas ng bioavailability kumpara sa karaniwang serum ng humigit-kumulang dalawang ikatlo ayon sa mga kamakailang pag-aaral noong nakaraang taon. Ang ganitong mapabuting paraan ng paghahatid ay nangangahulugan na ang mga pasyente ay maaaring gumaling nang walang cicatrisation kahit kapag nakikipaglaban sa mga matitigas na kronikong sugat na karaniwang lumalaban sa tradisyonal na paggamot.
Mga Hinaharap na Direksyon sa Biotherapy para sa Pagpapabalik ng Imyunidad ng Balat
Mga Nag-uumpisang Trend sa Tissue Engineering at Personalisadong Bio-Faktor
Ang mga mananaliksik ay nakakamit ng malalaking hakbang sa 3D bioprinting ng mga istruktura ng balat na talagang naglalaman ng tiyak na mga biological factor mula mismo sa mga pasyente, na tumutulong sa mas tumpak na pagbabago ng kanilang mga immune response. Ayon sa isang kamakailang pag-aaral na nailathala sa Advanced Healthcare Materials noong nakaraang taon, ang pagsasama ng mga espesyal na gel na tinatawag na bioactive hydrogels kasama ang isang bagay na tinatawag na phage therapy ay nagpapabilis sa paggaling ng mga sugat na may impeksyon ng humigit-kumulang 35%. Talagang kahanga-hangang impormasyon! Ang mga kasangkapan sa artipisyal na katalinuhan ay nagsisimula nang makialam dito, na tumutulong sa mga siyentipiko na malaman kung anong halo ng mga biological factor ang pinakaepektibo para sa iba't ibang immune system ng mga tao, lalo na yaong mga may kondisyon tulad ng psoriasis o lupus kung saan nilulusob ng katawan ang sarili nitong bahagi. Lahat ng ito ay tugma sa sinulat ng mga eksperto sa isang papel mula sa Frontiers in Bioengineering and Biotechnology na nailathala mas maaga ngayong taon, kung saan sila ay nagsabi na kailangan nating mapabuti ang paglikha ng mga customized na bersyon ng napakaliit na tagapaghatid ng mensahe sa selula na kilala bilang extracellular vesicles.
Mga hamon sa klinikal na pagsasalin at mga landas ng regulasyon
Bagaman malakas ang mga preklinikal na resulta, tanging 12% lamang ng mga terapiya gamit ang bio-factor ang nakarating sa ika-3 yugto ng pagsubok noong 2020–2023 dahil sa mga isyu sa standardisasyon. Ang mga ahensya ng regulasyon ay nangangailangan na ng masusing paglalarawan sa mga bahagi ng exosome, lalo na ang dala-dalang cytokine. Dagdag pa rito, ang mga pagkakaiba sa regulasyon sa iba't ibang bansa ay nagpapabagal pa sa pag-apruba, na nagpapakita ng pangangailangan para sa pinagsamang balangkas upang matiyak ang kaligtasan habang binibilisan ang komersyalisasyon.
Matalinong mga sistema ng paghahatid na tumutuon sa polarisasyon ng makrophage
Ang mga bagong biomimetic scaffolds ay isinasama na ngayon ang mga controlled release system na talagang tumutulong sa pagbabago ng macrophages mula sa kanilang nakapapanaig na estado na M1 patungo sa nakapagpapagaling na uri na M2. Ang ilang paunang pag-aaral ay tiningnan ang paggamit ng exosomes mula sa keratinocytes sa loob ng mga espesyal na pH-sensitive gels, at napansin ng mga mananaliksik na halos kalahating bilis na nalulutas ang chronic inflammation sa mga mouse model kumpara sa tradisyonal na pamamaraan. Mayroon ding isang napakainteresanteng papel na nailathala noong nakaraang taon sa APL Materials na nagpapakita kung paano pinapabuti ng pagdaragdag ng graphene oxide sa mga maliit na delivery vehicle ang pag-target sa tamang bahagi ng skin immune cells ng humigit-kumulang 72 porsiyento kumpara dati. Ang ganitong mapabuting targeting ay nangangahulugan ng mas kaunting hindi inaasahang reaksyon ng immune sa ibang bahagi ng katawan, na mahalaga sa praktikal na aplikasyon.
FAQ
Ano ang biotherapy sa dermatology?
Ang biotherapy sa dermatology ay gumagamit ng mga biological na sangkap, tulad ng mga protina at exosomes, upang tugunan ang mga problema sa balat tulad ng eksema at psoriasis sa pamamagitan ng pagta-target sa mga ugat na immune dysfunction.
Paano binabago ng mga bioactive na sangkap ang imunidad ng balat?
Ang mga bioactive na sangkap ay tumutulong sa pagbabalanse ng antas ng cytokine at nakakaapekto sa pag-uugali ng macrophage, kaya pinapabuti ang imunidad ng balat at pinalalakas ang proseso ng pagpapagaling.
Ano ang papel ng exosomes sa pangangalaga ng balat?
Ang mga exosome ay gumagana bilang mensahero na dala ang mga protina at RNA fragments sa pagitan ng mga selula, na tumutulong sa pagrepara ng pinsala sa balat at pagbawas ng oxidative stress.
Anong mga hamon ang kinakaharap ng mga biotherapy na paggamot sa klinikal na aplikasyon?
Ang mga hamon ay kinabibilangan ng standardisasyon ng mga bio-factor therapy at pag-navigate sa mga regulasyon, na nagdudulot ng pagkaantala sa malawakang paggamit.
Talaan ng mga Nilalaman
- Pag-unawa sa Biotherapy at ang Papel Nito sa Regulasyon ng Imyunong Balat
-
Mga Bio-factor at Inter-cellular na Komunikasyon sa Pamamagitan ng Extracellular Vesicles
- Mga Exosome sa Pagtanda ng Balat at Photoaging: Mga Mekanismo ng Inter-cellular na Pagpapadala ng Senyas
- Mga Exosome na Galing sa Stem Cell at ang Kanilang Potensyal na Terapeutiko sa Pagbabago ng Imapre
- Mesenchymal Stem Cells (MSCs) at Ang Kanilang Paracrine Effects sa Pagkukumpuni ng Balat
- Biomimetic Biomaterials na Pina-enhance ang Pagpapadala ng Extracellular Vesicle
- Mga Epekto sa Imyunomodulasyon ng mga Bio-factor sa Mga Nakakahawang Kondisyon ng Balat
- Mga Mahahalagang Growth Factor at Endogenous na Landas ng Pagkukumpuni ng Balat
- Mga Hinaharap na Direksyon sa Biotherapy para sa Pagpapabalik ng Imyunidad ng Balat
- FAQ

 EN
EN








































